Surgical technology involves the study and use of medical instruments to assist in surgical procedures․ It requires precision, knowledge of sterile techniques, and collaboration with surgical teams to ensure patient safety and effective outcomes․
Overview of Surgical Technology as a Profession
Surgical technology is a vital healthcare profession focused on assisting surgeons and surgical teams during procedures․ It requires specialized education and training in sterile techniques, instrument handling, and surgical procedures․ Surgical technologists play a critical role in maintaining the sterile field, preparing operating rooms, and ensuring the smooth execution of surgeries․ This profession demands precision, attention to detail, and strong teamwork skills to support patient care and surgical success․
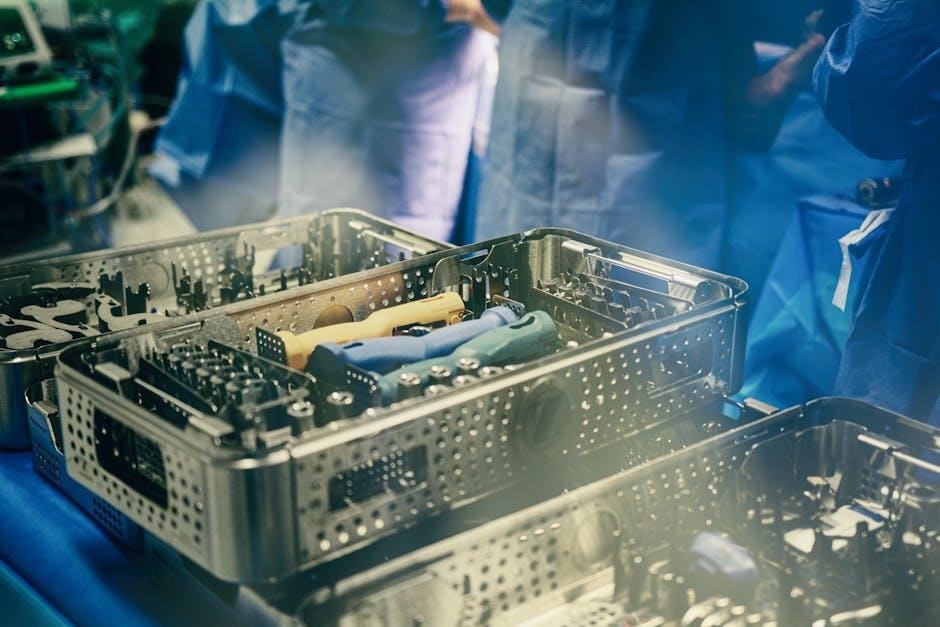
Importance of Surgical Instruments in Procedures
Surgical instruments are essential for achieving precise and safe outcomes in surgical procedures․ They enable surgeons to perform tasks with accuracy, from cutting and clamping to retracting and suturing․ Properly sterilized and maintained instruments prevent infections and ensure patient safety․ The role of surgical technologists in handling these tools is critical, as their expertise directly impacts the efficiency and success of surgical interventions, making them indispensable in the operating room environment․
Basic Surgical Instruments
Basic surgical instruments are fundamental tools used in surgical procedures, enabling tasks like cutting, dissecting, and retracting․ They are essential for surgeons and technologists to perform effectively․
Classification of Surgical Instruments
Surgical instruments are classified based on their functions and purposes in procedures․ Common categories include cutting instruments (e․g․, scalpels, scissors), clamping instruments (e․g․, forceps, clamps), retracting instruments (e․g․, retractors, suction tubes), and suturing tools․ This classification helps in organizing and selecting the appropriate tools for specific tasks, ensuring efficiency and precision during surgeries․ Understanding these categories is essential for surgical technologists to prepare and handle instruments effectively, maintaining sterility and workflow in the operating room․
Cutting Instruments: Scalpels and Scissors
Cutting instruments, such as scalpels and surgical scissors, are essential for making precise incisions and cutting tissues during procedures․ Scalpels typically consist of a handle and interchangeable blades, with sizes like #10, #11, #15, and #20, each designed for specific tasks․ Surgical scissors, available in straight or curved styles, are used for cutting sutures, tissues, or other materials․ Proper handling and knowledge of these tools are critical for surgical technologists to ensure efficient and safe surgical outcomes․
Clamping Instruments: Forceps and Clamps
Clamping instruments, such as forceps and clamps, are used to hold tissues, blood vessels, or objects in place during surgery․ Forceps, like needle holders, are used for gripping small items, while clamps, such as Kelly or Allis clamps, are used to control bleeding or secure tissues․ These tools are vital for maintaining hemostasis and providing traction, ensuring precise surgical control․ Proper selection and handling of clamps and forceps are essential for surgical technologists to support surgeons effectively during procedures․
Retracting Instruments: Retractors and Suction Tubes
Retractors and suction tubes are crucial for exposing surgical sites and maintaining a clear field․ Retractors, such as Deaver or Bookwalter retractors, gently pull back tissues to enhance visibility, while suction tubes remove fluids and debris․ Proper use of these tools by surgical technologists ensures optimal visualization for surgeons, promoting efficient and safe procedures․ Effective management of retractors and suction tubes is essential for minimizing complications and maintaining surgical site integrity․
Suturing and Stapling Instruments
Suturing and stapling instruments are essential for closing incisions and securing tissues during surgery․ Common tools include needle holders, surgical staplers, and suture scissors․ Needle holders are used to grasp and maneuver sutures, while staplers apply metal staples to quickly close wounds․ Proper handling ensures precise tissue closure and minimizes complications․ These instruments are vital for achieving effective wound closure, promoting healing, and maintaining surgical site integrity․ Their correct use is a critical skill for surgical technologists to master․

Sterile Technique and Instrument Handling
Sterile technique ensures instruments remain contamination-free, crucial for preventing surgical site infections․ Proper handling involves correct gowning, gloving, and maintaining asepsis throughout procedures to safeguard patient safety․
Principles of Sterile Technique
Sterile technique is fundamental in surgical settings to prevent infections․ It involves creating and maintaining asepsis, ensuring all instruments and surfaces are free from pathogens․ Proper handwashing, donning sterile gowns and gloves, and avoiding contamination are critical․ Traffic control in the OR limits exposure, and all team members must adhere to strict protocols․ These principles ensure a safe environment for patients and optimal surgical outcomes․ Continuous training reinforces these essential practices․
Proper Handling of Surgical Instruments
Proper handling of surgical instruments ensures safety and efficiency during procedures․ Instruments must be held and passed carefully to avoid damage or injury․ Using the correct technique for passing sharp objects, such as scalpels, is crucial to prevent accidents․ Maintaining sterility by handling instruments only with gloved hands and keeping them organized on the Mayo stand is essential․ Regular inspection and proper storage after procedures extend the lifespan of instruments and uphold surgical standards․
Maintaining Sterility During Procedures
Maintaining sterility is critical to prevent infections and ensure patient safety․ The surgical team must adhere to strict protocols, including proper gowning, gloving, and controlling OR traffic․ Instruments and supplies must be sterilized and handled only within the sterile field․ Any breach in sterility must be addressed immediately to minimize contamination risks․ Continuous vigilance by the surgical technologist ensures the sterile environment is preserved throughout the procedure, safeguarding both the patient and surgical team․

The Surgical Team and Roles
The surgical team is a collaborative group of professionals working together to ensure safe and efficient procedures․ It includes surgeons, anesthesiologists, nurses, and surgical technologists, each with distinct responsibilities to support patient care and surgical outcomes․
Understanding the Surgical Team Structure
The surgical team structure is a well-defined hierarchy ensuring efficient collaboration during procedures․ It includes surgeons, anesthesiologists, nurses, and surgical technologists, each playing a critical role․ Surgeons perform the operation, while anesthesiologists manage patient anesthesia․ Nurses assist with patient care and maintain the surgical environment, and technologists handle instruments and equipment․ This interdependent structure ensures clear communication, accountability, and seamless execution of surgical procedures, ultimately prioritizing patient safety and optimal outcomes․
Role of the Surgical Technologist
The surgical technologist plays a vital role in ensuring the smooth progression of surgical procedures․ Their primary responsibilities include preparing the operating room, sterilizing equipment, and arranging surgical instruments․ During surgery, they assist the surgeon by handing instruments, maintaining a sterile field, and managing supplies․ They also monitor patient safety, handle sharp instruments, and ensure proper counting of sponges and instruments․ Their expertise in surgical instrumentation and sterile technique is crucial for maintaining operative efficiency and patient care․
Surgeon, Anesthesiologist, and Nurse Roles
The surgeon performs the operation, making precise incisions and executing the surgical plan․ The anesthesiologist ensures patient comfort and safety by administering anesthesia and monitoring vital signs․ Nurses assist with patient preparation, maintain the sterile field, and provide post-operative care․ Each role is critical, requiring collaboration to ensure optimal patient outcomes and a smooth surgical process․

Surgical Instrument Care and Maintenance
Proper cleaning, disinfection, and storage of surgical instruments are essential to maintain their functionality and prevent contamination․ Regular maintenance ensures longevity and readiness for procedures․
Cleaning and Disinfection of Instruments
Cleaning and disinfection of surgical instruments are critical to prevent contamination and ensure patient safety․ Instruments must be thoroughly cleaned using enzymatic solutions and ultrasonic cleaners before disinfection․ High-level disinfection methods, such as autoclaving or chemical vapor, are applied to destroy pathogens․ Proper rinsing and drying are essential to maintain instrument quality․ Following manufacturer guidelines ensures effective disinfection and longevity of instruments, adhering to strict infection control protocols․ This process is vital for maintaining sterility and preventing surgical site infections․
Storage and Organization of Surgical Instruments
Proper storage and organization of surgical instruments are essential for maintaining sterility and functionality․ Instruments should be stored in protective cases or pouches to prevent damage and corrosion․ They must be organized by type, size, or procedure to ensure quick access during surgeries․ Labeling and categorizing instruments help in easy identification and retrieval․ Storage areas should be clean, dry, and climate-controlled to preserve instrument quality․ Proper organization enhances efficiency and safety in surgical settings, ensuring all tools are readily available and in optimal condition for use․
Troubleshooting Common Instrument Malfunctions
Troubleshooting instrument malfunctions involves identifying issues like dull blades, loose handles, or corrosion․ Regular maintenance and inspection are key to preventing problems․ If an instrument fails during surgery, it should be removed and replaced promptly․ Technicians must follow repair protocols or seek professional assistance․ Proper documentation of malfunctions ensures accountability and future prevention․ Swift resolution minimizes delays, maintaining surgical efficiency and patient safety․ Understanding common issues helps surgical technologists act decisively, upholding the standard of care․

Specialized Surgical Instruments
Specialized instruments are designed for specific surgical fields, such as cardiothoracic, orthopedic, or laparoscopic procedures․ They require precise handling and training to ensure optimal performance and patient outcomes․
Cardiothoracic and Vascular Instruments
Cardiothoracic and vascular instruments are highly specialized tools used in surgeries involving the heart, lungs, and blood vessels․ These include bulldog clamps, Cooley clamps, and vascular staplers․ Designed for precision, they often feature fine tips and ergonomic handles to minimize tissue damage․ Materials like titanium and stainless steel ensure durability and compatibility with sterilization methods․ These instruments are critical in procedures such as coronary artery bypass grafting and aneurysm repairs, requiring meticulous handling to maintain patient safety and surgical success․
Orthopedic and Neurosurgical Instruments
Orthopedic and neurosurgical instruments are designed for precision in surgeries involving bones, joints, and the nervous system․ Common tools include bone cutters, nerve retractors, and spinal dissectors․ Neurosurgical instruments like suction tubes and aneurysm clips are used for delicate brain procedures․ Orthopedic instruments, such as fracture reduction forceps, assist in stabilizing bones․ These tools are typically made from stainless steel or titanium, ensuring durability and sterility․ Proper handling and sterilization are crucial for successful patient outcomes in these specialized surgical fields․
Laparoscopic and Endoscopic Instruments
Laparoscopic and endoscopic instruments enable minimally invasive surgeries, reducing recovery time․ Key tools include trocars, laparoscopic graspers, and endoscopic cameras․ These instruments allow visualization of internal organs through small incisions․ Specialized tools like dissectors and cautery devices facilitate precise tissue manipulation․ Endoscopic instruments, such as biopsy forceps, are used for diagnostic procedures․ Proper sterilization and handling are essential to maintain the integrity of these delicate instruments, ensuring safe and effective patient care during minimally invasive surgical procedures․
Surgical Patient Preparation
Surgical patient preparation involves cleaning the surgical site, positioning the patient, and draping to maintain sterility․ Proper preparation ensures a safe and effective surgical environment for the procedure․
Preparation of the Patient for Surgery
Preparation of the patient for surgery involves assessing their medical history, ensuring proper hygiene, and positioning them correctly on the operating table․ This step is critical to ensure safety and comfort during the procedure․ The surgical technologist plays a key role in maintaining a sterile environment and preparing the patient according to established protocols․ Proper draping and positioning are essential to prevent complications and facilitate smooth surgical operations․ Attention to detail ensures the patient is ready for a successful procedure․
Positioning the Patient on the Operating Table
Proper patient positioning on the operating table is essential for ensuring access to the surgical site and preventing complications․ Surgical technologists play a critical role in positioning patients safely, using techniques that align with the procedure’s requirements․ This includes adjusting the table’s height and angle, and securing the patient with padding or straps to maintain stability․ Correct positioning minimizes the risk of nerve damage, promotes optimal surgical exposure, and ensures patient safety throughout the procedure․ Precision is key to achieving these goals effectively․
Draping Techniques and Maintaining the Sterile Field
Draping techniques are critical for creating and maintaining a sterile field during surgery․ Surgical technologists use disposable drapes to cover the patient and operating table, ensuring only the surgical site is exposed․ The sterile field’s boundaries must be clearly defined to prevent contamination․ Team members must avoid reaching over the field and ensure all instruments are placed within its boundaries․ Proper draping and adherence to sterile protocols are essential for minimizing infection risks and maintaining a safe surgical environment throughout the procedure․

Surgical Count Procedures
Surgical count procedures ensure all instruments are accounted for during procedures, preventing loss and maintaining patient safety․ They involve counting before, during, and after surgery, with documentation and team coordination to uphold sterility and organization․
Importance of Instrument and Sponge Counts
Instrument and sponge counts are critical for patient safety, preventing retained objects and complications․ They ensure all items are accounted for, maintaining sterility and organization․ Counts verify equipment integrity, reduce risks, and promote team coordination, ensuring accurate documentation and adherence to protocols․ This process is vital for legal compliance and upholding surgical standards, protecting both patients and healthcare providers from potential errors and consequences․ Accurate counts are a cornerstone of surgical integrity and efficiency․
Handling Sharp Instrument Counts
Handling sharp instrument counts requires meticulous attention to prevent retained objects․ Counting before and after procedures ensures all sharps are accounted for, reducing risks of injury or complications․ Use designated containers and follow strict protocols to maintain sterility and organization․ Double-counting by two team members enhances accuracy․ Communication and documentation are critical to ensure patient safety and compliance with surgical standards․ This process minimizes errors and upholds surgical integrity while protecting both patients and staff from potential harm․
Protocols for Missing or Mismatched Counts
When counts are mismatched or instruments are missing, immediate action is required․ Conduct a thorough search of the surgical site and linens․ Use X-ray detection if necessary․ Document the issue and notify the surgical team․ Follow facility protocols for reporting discrepancies․ Ensure patient safety by verifying all items are accounted for before concluding the procedure․ Maintain accurate records and review the incident to prevent future occurrences, upholding surgical standards and patient care integrity․
Anesthesia and Patient Monitoring
Anesthesia ensures patient comfort and safety during surgery․ Surgical technologists assist in monitoring vital signs and maintaining anesthesia equipment, crucial for optimal surgical outcomes and patient care․
Basic Principles of Anesthesia in Surgery
Anesthesia ensures patient comfort and safety by preventing pain and discomfort during surgery․ It involves assessing the patient’s health, administering medications, and monitoring vital signs․ Surgical technologists assist by preparing anesthesia equipment and supplies․ The primary goal is to maintain patient stability, ensuring proper airway management, breathing, and circulation․ Effective communication between the anesthesiologist and surgical team is critical for safe anesthesia administration and monitoring throughout the procedure․
Role of the Surgical Technologist in Anesthesia
The surgical technologist plays a crucial role in anesthesia by preparing and organizing equipment, ensuring all devices are functional and sterile․ They assist the anesthesiologist by maintaining supplies, monitoring equipment, and providing necessary instruments during procedures․ Their attention to detail ensures patient safety and efficient anesthesia administration․ Collaboration with the anesthesia team is vital to anticipate needs and maintain a seamless workflow during surgical procedures․
Patient Monitoring During Surgical Procedures
Patient monitoring is critical during surgery to ensure safety and optimal outcomes․ Surgical technologists assist in monitoring vital signs, such as heart rate and blood pressure, using specialized equipment․ They also observe anesthesia levels and prepare for potential complications․ Their role includes maintaining a sterile environment and handling instruments to ensure the procedure remains seamless․ Effective monitoring allows the surgical team to respond promptly to any changes, ensuring the patient’s well-being throughout the operation․

Emergencies in the Operating Room
Emergencies require prompt action to ensure patient safety․ Surgical fires, cardiac arrests, and complications demand quick responses․ The surgical team must act swiftly to manage crises effectively․
Handling Surgical Fires and Emergencies
Surgical fires and emergencies require immediate action to ensure patient safety․ Prevention involves proper use of flammable materials and electrical equipment․ In case of a fire, the surgical team must remain calm, isolate the fire source, and evacuate if necessary․ Fire extinguishers and emergency protocols should always be accessible․ Clear communication and quick decision-making are critical to managing crises effectively and minimizing risks during procedures․
Managing Patient Complications During Surgery
Managing patient complications during surgery requires vigilance and quick action․ Surgical technologists must monitor for signs of adverse reactions, such as bleeding or respiratory distress․ They assist in preparing emergency instruments and medications, ensuring the surgical team can address issues promptly․ Effective communication and adherence to established protocols are critical to minimizing risks and ensuring patient safety during unexpected events․
Protocols for Cardiac Arrest in the OR
Cardiac arrest in the OR demands immediate action․ Surgical technologists must activate the emergency response system and prepare defibrillators and medications․ They assist in securing the airway and preparing for chest compressions while maintaining sterility․ Collaboration with the anesthesia team is crucial to ensure proper ventilation and medication administration․ Protocols prioritize patient stabilization, adhering to ACLS guidelines, and clear communication to minimize delays and improve outcomes during this high-stakes situation․
Career Development for Surgical Technologists
Advancement in surgical technology involves certification, specialized training, and continuous professional development․ Pursuing CST certification and staying updated on industry advancements are key to career growth and excellence․
Certification and Licensure Requirements
Certification and licensure are critical for surgical technologists to demonstrate competency and professionalism․ The Certified Surgical Technologist (CST) credential, offered by the National Board of Surgical Technology and Surgical Assisting (NBSTSA), is a key requirement․ Many employers mandate this certification, which involves passing an exam and completing continuing education․ Additionally, licensure requirements vary by state, with some requiring registration or specific certifications․ Accreditation by the Commission on Accreditation of Allied Health Education Programs (CAAHEP) ensures program quality, making it essential for eligibility to sit for the CST exam․
- CAAHEP-accredited programs are necessary for CST eligibility․
- CST certification demonstrates expertise and commitment to the field․
- State licensure requirements vary, so checking local regulations is crucial․
Specializations and Advanced Roles
Surgical technologists can pursue specialized roles in cardiothoracic, neurosurgery, or orthopedic fields, requiring expertise in specific instruments․ Advanced roles include surgical first assistants, instrument managers, or educators․ These positions demand additional training and certifications, such as the Certified Surgical First Assistant (CSFA) credential․ Specialization allows technologists to deepen their expertise, enhancing career growth and opportunities in high-demand surgical specialties․
- Specialized roles require advanced certifications and training․
- Expertise in specific surgical fields increases career opportunities․
- Leadership roles, like instrument management, are available for experienced technologists․
Continuous Professional Development
Continuous professional development is crucial for surgical technologists to stay updated on advancements in surgical techniques and instrumentation․ This involves attending workshops, pursuing further certifications, and engaging in lifelong learning․ Technologists must maintain certifications like CST and stay informed about new technologies․ Practical training and exposure to specialized procedures enhance skills and adaptability in the evolving surgical landscape, ensuring patient safety and advancing one’s career prospects․
- Stay updated with advancements in surgical techniques․
- Pursue certifications and ongoing education․
- Engage in practical training and workshops․
Mastery of surgical instruments and techniques is essential for ensuring patient safety and successful outcomes․ Continuous learning and adaptation to advancements are key to professional growth and excellence․
Summarizing Key Concepts
Mastering surgical instruments and understanding their proper use is critical for surgical technologists․ Key concepts include maintaining sterility, handling instruments safely, and anticipating the surgeon’s needs․ The surgical team’s interdependence and effective communication are vital for successful procedures․ Continuous learning and adapting to new technologies ensure proficiency․ Proper instrument care, from cleaning to storage, prevents malfunctions and extends longevity․ By understanding these principles, surgical technologists play a pivotal role in ensuring patient safety and optimal surgical outcomes․
Final Thoughts on Mastering Surgical Instruments
Mastering surgical instruments requires dedication, continuous learning, and a deep understanding of their roles in procedures․ Proper handling, sterility, and anticipation of the surgeon’s needs are essential skills․ Staying updated on advancements and maintaining precise techniques ensure efficiency and safety․ By prioritizing instrument care and collaboration with the surgical team, technologists contribute significantly to successful outcomes and patient well-being, fostering a culture of excellence in surgical practice and professional growth․